State of the Art
Medical and Surgical Care Near You
Placing you and your safety at the heart of everything we do
About
Dr. Steven J Hillam
Dr. Hillam is a board-certified ophthalmologist and fellow of the American Osteopathic College of Ophthalmology.
He was born and raised in Provo, UT where he graduated from Brigham Young University. He completed his medical degree at the Kirksville College of Osteopathic Medicine in 2011.
Following medical school, Dr. Hillam relocated his family to the state of Michigan where he joined the Consortium of Osteopathic Residents in Ophthalmology (CORO) at Michigan State University and completed his internship and residency through Beaumont hospitals in Taylor, Michigan.
Dr. Hillam comes to us from New Mexico where he performed more than 700 cataract surgeries per year and thousands of treatments for diabetes, glaucoma and macular degeneration. He is excited to be back in the area he proudly calls home.
Eye Health and Vision

Cataracts
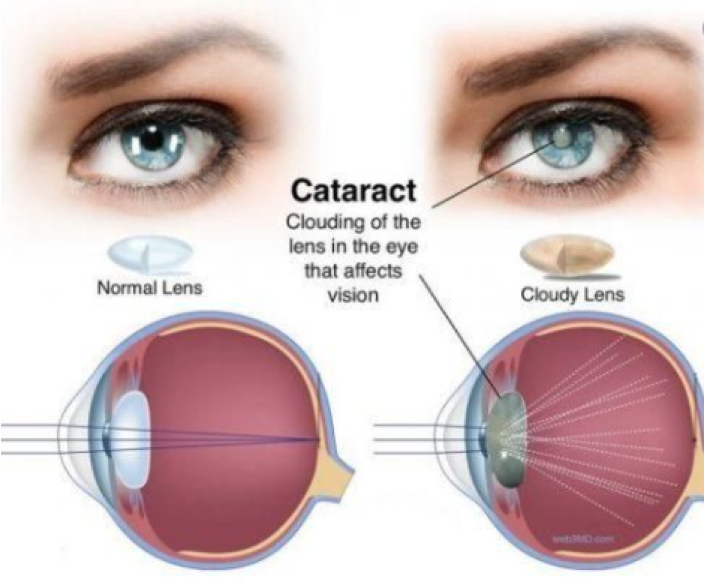
A Cataract is a clouding of the natural lens inside the eye, hindering the eye’s ability to focus properly.

Diabetic Eye Disease
Diabetes is a disease that affects the body’s ability to produce or use insulin effectively to control blood sugar (glucose) levels.

Glaucoma
Glaucoma is one of the leading causes of blindness for people over 60 years old. Thankfully, blindness from glaucoma can often be prevented with early treatment.

Macular Degeneration
Age-related macular degeneration (AMD) is very common. It is a leading cause of vision loss in people 50 years or older.
Don't Compromise Your Eyes
Client Reviews
What Is Diabetes?
Diabetes is a disease that affects the body’s ability to produce or use insulin effectively to control blood sugar (glucose) levels. Too much glucose in the blood for a long time can cause damage throughout the body. Diabetes directly damages the heart, kidneys and blood vessels. It directly effects the small blood vessels in the eye. Even if diabetes is well controlled, it can still affect your regular eye care.
The Centers for Disease Control and Prevention (CDC) says that about 90% of vision loss from diabetes can be prevented. Early detection is key. It is critical that people with diabetes should get annual eye exams even before they have signs of vision loss. Studies show that 60% of diabetics are not getting the exams their doctors recommend.
What Is Diabetic Eye Disease?
Diabetic eye disease is a term for several eye problems that can all result from diabetes. Diabetic eye disease includes:
- diabetic retinopathy
- diabetic macular edema
- cataract
- glaucoma
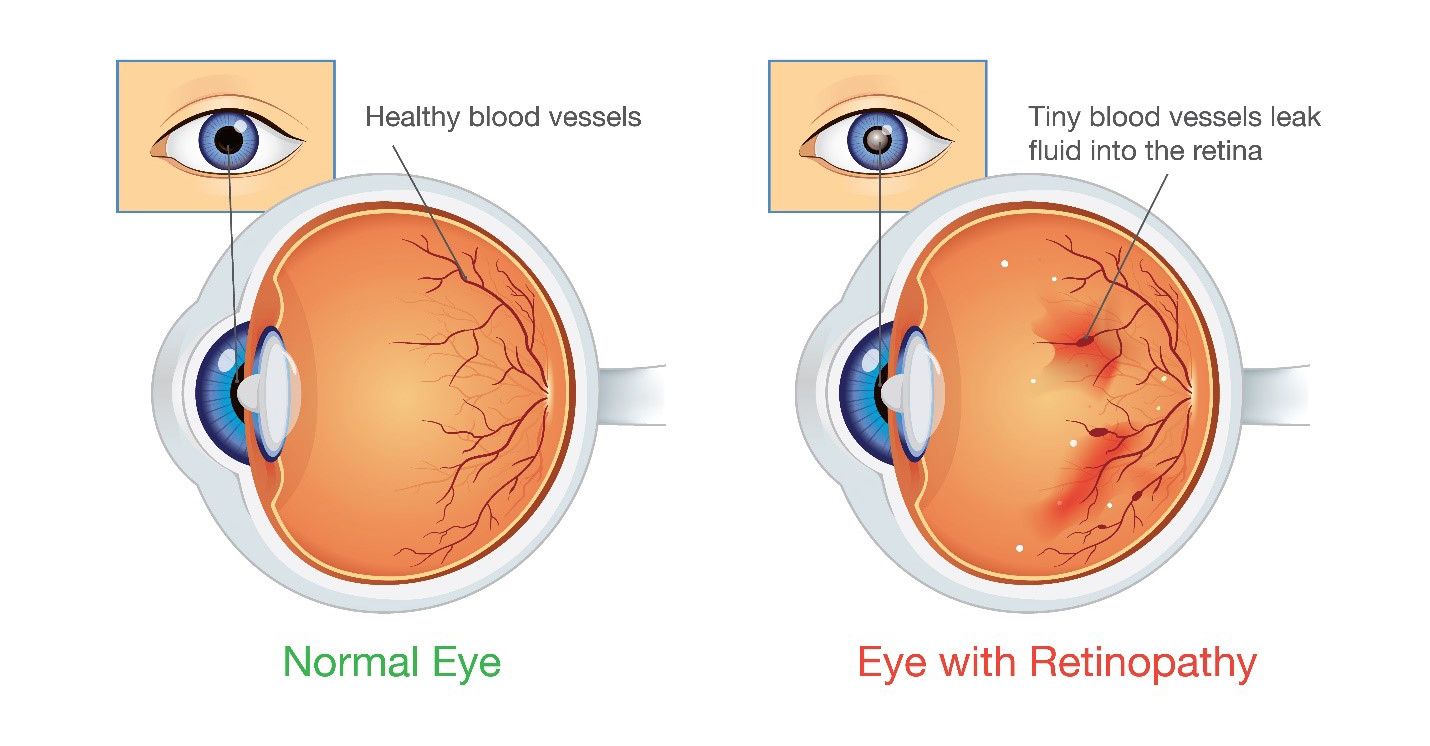
Diabetic retinopathy
Diabetic retinopathy is a condition when diabetes causes blood vessels in the retina to swell, leak or close off completely. As a result, abnormal new blood vessels can also grow on the surface of the retina.
People who have diabetes or poor blood sugar control are at risk for diabetic retinopathy. Risk also increases the longer someone has diabetes.
Diabetic macular edema
Macular edema happens when fluid builds up in the Macula (the portion of the retina responsible for detailed central vision) and causes swelling and blurry vision. Diabetes can cause macular edema. Diabetic macular edema can lead to permanent vision loss.
Diabetes and cataracts
Excess blood sugar from diabetes can cause cataracts to develop more rapidly than normal. You may need cataract surgery to remove lenses that are clouded by the effects of diabetes. Maintaining good control of your blood sugar helps prevent permanent clouding of the lens and the need for surgery.
Diabetes and glaucoma
Glaucoma is a group of diseases that cause damage to your eye's optic nerve. This damage leads to irreversible loss of vision. Having diabetes doubles your chance of getting glaucoma.
Other Eye Problems Are Related to Diabetes
Diabetes can cause vision problems even if you do not have a form of diabetic eye disease. These can include:
- Blurry vision. If your blood sugar levels change quickly, it can affect the shape of the lens inside your eye, causing blurry vision. Your vision usually goes back to normal after your blood sugar stabilizes. It is important to have good blood sugar control before getting your eyeglasses prescription checked. This ensures you receive the correct prescription.
- Double vision. Diabetes can damage the nerves that move the eyes and help them work together. This nerve damage can cause double vision.
- Diabetes is a risk factor for other eye diseases, including Branch Retinal Vein Occlusion (BRVO), and Central Retinal Vein Occlusion (CRVO). These can be very devastating to your vision.
Diagnosis
Diabetic retinopathy is best diagnosed with a comprehensive dilated eye exam. For this exam, drops placed in your eyes widen (dilate) your pupils to allow the doctor a better view inside your eyes. The drops make you sensitive to bright light, and can cause your close vision to blur until they wear off, which usually takes several hours.
During the exam, your eye doctor will look for diabetes-related abnormalities on the inside and outside areas of your eyes.
An Optical Coherence Tomography (OCT) may be performed as part of the exam. This advanced technology provides cross-sectional images of the retina that show the layers of the retina. This helps determine how much fluid, if any, has leaked into the retina tissue. Later, OCT exams can be used to monitor how treatment is working.
Treatment
Treatment of Diabetic Eye Disease is geared toward slowing or stopping the progression its effects, which depends largely on the type and severity of diabetic retinopathy you have.
Early diabetic retinopathy
If you have mild or moderate Non-Proliferative Diabetic Retinopathy (NPDR), you might not need treatment right away. However, your eye doctor will closely monitor your eyes to determine when/if you might need treatment. Regular eye exams will help your ophthalmologist detect and treat potentially vision-threatening problems before they become devastating to your vision. Also work with your diabetes doctor or endocrinologist to determine if there are ways to improve your diabetes management. When diabetic retinopathy is mild or moderate, good blood sugar control can usually be sufficient to slow the progression of diabetic retinopathy.
Advanced diabetic retinopathy
If you have the more advanced Proliferative Diabetic Retinopathy (PDR) or Diabetic Macular Edema, you'll need prompt treatment. Depending on the specific problems with your retina, treatment options might include:
- Injections of medications into the eye
These medications, called Vascular Endothelial Growth Factor inhibitors (anti-VEGF), are injected into the vitreous through the wall of the eye. They are very effective in helping to stop the growth of new blood vessels and decrease fluid buildup. These drugs are injected after using topical anesthesia. Although it sounds intimidating, the injections are usually tolerated quite well by the patient. The injections can cause mild discomfort, such as burning, tearing or achiness, for a few minutes to 24 hours after the injection. Possible side effects include a temporary increase of pressure in the eye and infection. These injections will need to be repeated. In some cases, the medication is used in combination with laser photocoagulation.
Currently two anti-VEGF drugs are approved by the U.S. Food & Drug Administration (FDA) for treatment of diabetic macular edema:
-
- Ranibizumab (Lucentis)
- Aflibercept (Eylea)
- A third drug, Bevacizumab (Avastin), is often an effective medication, but has not been approved by the FDA for this specific application. However, it can also be used off-label for the treatment of diabetic macular edema.
- Photocoagulation
This laser treatment, also known as focal laser treatment, can stop or slow the leakage of blood and fluid in the eye. During the procedure, leaks from abnormal blood vessels are treated with laser burns. Focal laser treatment is usually done in your doctor's office or eye clinic in a single session. If you had blurred vision from macular edema before surgery, the treatment might not return your vision to normal, but it is likely to reduce the chance of the macular edema worsening.
- Pan-retinal Photocoagulation
This laser treatment, also known as scatter laser treatment, can shrink the problematic abnormal blood vessels. During the procedure, the areas of the retina away from the macula are treated with scattered laser burns. The treated spots cause the problematic new blood vessels to shrink and scar. It is usually done in your doctor's office or eye clinic in two or more sessions. It is normal for your vision to be blurry for about a day after the procedure. A decrease of peripheral vision or night vision after the procedure is possible.
- Vitrectomy
In the case of a severe hemorrhage caused by diabetes, a Vitrectomy is a surgical procedure that can be utilized to remove the blood from the middle of the eye (vitreous). It is done in a surgery center or hospital using local or general anesthesia.
While treatment can slow or stop the progression of diabetic retinopathy, it is not a cure. Because diabetes is a lifelong condition, future retinal damage and vision loss are still possible. Even after successful treatment for diabetic retinopathy, you'll need regular eye exams. The effects of diabetes are different for every individual, and at some point, you may need additional treatment.
Take Steps to Protect Your Vision
To prevent eye damage from diabetes, maintain good control of your blood sugar. Follow your primary care physician's diet and exercise plan. If you have been diagnosed with Diabetes or Pre-Diabetes and have not had an eye exam with an ophthalmologist, it is crucial to get one now. Be sure to never skip the follow-up exams that your ophthalmologist recommends.
Glaucoma
Glaucoma is one of the leading causes of blindness for people over 60 years old. Thankfully, blindness from glaucoma can often be prevented with early treatment.
The Effects Glaucoma
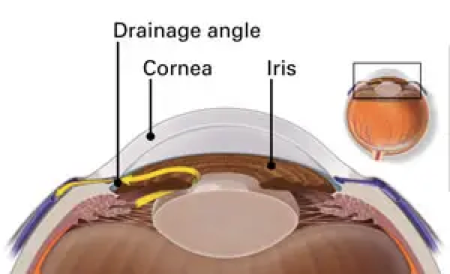
The tissues inside the eye are constantly producing a watery fluid called aqueous humor. As new aqueous flows into your eye, the same amount needs to drain out. The fluid drains out through an area called the drainage angle and is absorbed by other body tissues around the eye. This process keeps pressure in the eye (called intraocular pressure or IOP) stable. But if the drainage angle doesn’t keep up with the amount of fluid produced inside the eye,
pressure inside the eye rises, damaging the optic nerve.
The optic nerve is made of more than a million tiny nerve fibers. It is like an electric cable made up of many small wires. As these nerve fibers are damaged and die, you will develop blind spots in your vision. Blind spots caused by Glaucoma usually effect the peripheral vision first, so you may not notice these blind spots until most of your optic nerve fibers have died. If all of the fibers die, you will become blind.
Glaucoma is a silent thief of sight
Glaucoma has no symptoms in its early stages. In fact, half the people with glaucoma do not know they have it! Having regular eye exams can help your ophthalmologist find this disease before you lose vision. Your ophthalmologist can tell you how often you should be examined.
How Do You Get Glaucoma?
There are two major types of Glaucoma:
- Primary open-angle glaucoma
This is the most common type of glaucoma. It happens gradually, where the eye does not drain fluid as well as it should (like a clogged drain). As a result, eye pressure builds and starts to damage the optic nerve. This type of glaucoma is painless and causes no noticeable vision changes at first.
Some people can have optic nerves that are sensitive to normal eye pressure. This means their risk of getting glaucoma is higher than usual. Regular eye exams are important to find early signs of damage to the optic nerve.
- Angle-closure glaucoma (also called “closed-angle glaucoma” or “narrow-angle glaucoma”)
This type happens when someone’s iris is very close to the drainage angle in their eye. The iris can crowd and block the drainage angle. You can think of it like a piece of paper sliding over a sink drain. When the drainage angle gets completely blocked, eye pressure rises very quickly. This is called an acute attack. It is a true eye emergency, and you should call your ophthalmologist right away or you might go blind.
These are the signs of an acute angle-closure glaucoma attack:
- Your vision is suddenly blurry
- You have severe eye pain
- You have a headache
- You feel sick to your stomach (nausea)
- You throw up (vomit)
- You see rainbow-colored rings or halos around lights
Many people with angle-closure glaucoma develop it slowly. This is called chronic angle-closure glaucoma. There are no symptoms at first, so they don’t know they have it until the damage is severe or they have an attack.
Angle-closure glaucoma can cause blindness if not treated right away.
Symptoms of Glaucoma
Open-angle glaucoma:
With the more common open-angle glaucoma, there are no warning signs or obvious symptoms in the early stages. As the disease progresses, blind spots develop in your peripheral (side) vision.
Most people with open-angle glaucoma do not notice any change in their vision until the damage is quite severe. This is why glaucoma is called the “silent thief of sight.” An Ophthalmologist can detect the condition, so having regular eye exams can help find the disease before you lose vision. Your ophthalmologist can tell you how often you should be examined based on findings during the exam.
Angle-closure glaucoma:
People at risk for angle-closure glaucoma usually show no symptoms before an attack. Some early symptoms of an attack may include blurred vision, halos, mild headaches or eye pain. People with these symptoms should be checked by an Ophthalmologist as soon as possible. An attack of angle-closure glaucoma includes the following:
- severe pain in the eye or forehead
- redness of the eye
- decreased vision or blurred vision
- seeing rainbows or halos
- headache
- nausea
- vomiting
Normal Tension Glaucoma:
You can have glaucoma and also have an intraocular pressure that is in the ‘normal’ range when tested. People with "normal tension glaucoma" have eye pressure that is within normal ranges, but show signs of glaucoma, such as blind spots in their field of vision and optic nerve damage. Like Open-Angle Glaucoma, this type can only be detected in the early stages with a proper eye exam.
What is “Glaucoma Suspect”?
Some people have no signs of damage but have higher than normal eye pressure (called ocular hypertension). These patients are considered "glaucoma suspects" and have a higher risk of eventually developing glaucoma. Some people are considered glaucoma suspects even if their eye pressure is normal. For example, their ophthalmologist may notice something different about their optic nerve. Most glaucoma suspects have no symptoms. That is why you need to be carefully monitored by an ophthalmologist if you are a glaucoma suspect. By nature, glaucoma advances, or worsens over time. An ophthalmologist can check for any changes over time and begin treatment if needed.
Pigment Dispersion Syndrome and Pigmentary Glaucoma:
Pigment dispersion syndrome (PDS) happens when pigment debris rubs off the back of your iris. This pigment can clog the drainage structures of the eye, raise eye pressure and lead to pigmentary glaucoma. Some people with PDS or pigmentary glaucoma may see halos or have blurry vision after activities like jogging or playing basketball. See your ophthalmologist if you have these or other symptoms.
Who Is at Risk for Glaucoma?
Some people have a higher-than-normal risk of getting glaucoma. This includes people who:
- are over age 40
- have family members with glaucoma
- are of African, Hispanic, or Asian heritage
- have high eye pressure
- are farsighted or nearsighted
- have had an eye injury
- use long-term steroid medications
- have corneas that are thin in the center
- have thinning of the optic nerve
- have diabetes, migraines, high blood pressure, poor blood circulation or other health problems affecting the whole body
Talk with an ophthalmologist about your risk for getting glaucoma. People with more than one of these risk factors have an even higher risk of glaucoma.
Glaucoma Diagnosis
The only sure way to diagnose glaucoma is with a complete eye exam. A glaucoma screening that only checks eye pressure is not enough to find glaucoma.
During a glaucoma exam, your ophthalmologist may:
- measure your eye pressure
- inspect your eye's drainage angle
- examine your optic nerve for damage
- test your peripheral (side) vision
- take a picture or computer measurement of your optic nerve
- measure the thickness of your cornea

Glaucoma Treatment
Damage to the eye from Glaucoma is permanent—it cannot be reversed. But medicine and surgery (if needed) help to stop further damage. To treat glaucoma, your ophthalmologist may use one or more of the following treatments.
- Medication
Glaucoma is usually controlled with medicine in the form of eyedrops. Used every day, these eye drops lower eye pressure. Some do this by reducing the amount of aqueous fluid the eye makes. Others reduce pressure by helping fluid flow better through the drainage angle.
Glaucoma medications can help you keep your vision, but they may also produce side effects. Some glaucoma eye drops may cause:
- a stinging or itching sensation
- red eyes or red skin around the eyes
- changes in your pulse and heartbeat
- changes in your energy level
- changes in breathing (especially if you have asthma or breathing problems)
- dry mouth
- blurred vision
- eyelash growth
- changes in your eye color, the skin around your eyes or eyelid appearance
All medications can have side effects. Some drugs can cause problems when taken with other medications. It is important to give your doctor a list of every medicine you take regularly. Be sure to talk with your ophthalmologist if you think you may have side effects from glaucoma medicine.
Never change or stop taking your glaucoma medications without talking to your ophthalmologist first. If you are about to run out of your medication, ask your ophthalmologist if you should have your prescription refilled.
- Laser surgery
There are two main types of laser surgery to treat glaucoma. They help aqueous drain from the eye. These procedures are usually done in the ophthalmologist’s office or an outpatient surgery center.
- Laser Trabeculoplasty
This surgery is for people who have open-angle glaucoma and can be used instead of or in addition to medications. The eye surgeon uses a laser to make the drainage angle work better. That way fluid flows out properly and eye pressure is reduced.
- Laser Iridotomy
This is for people who have angle-closure glaucoma. The ophthalmologist uses a laser to create a tiny hole in the iris. This hole helps fluid flow to the drainage angle.
- Surgery in the operating room
Some glaucoma surgery is done in an operating room. It creates a new drainage channel for the aqueous humor to leave the eye.
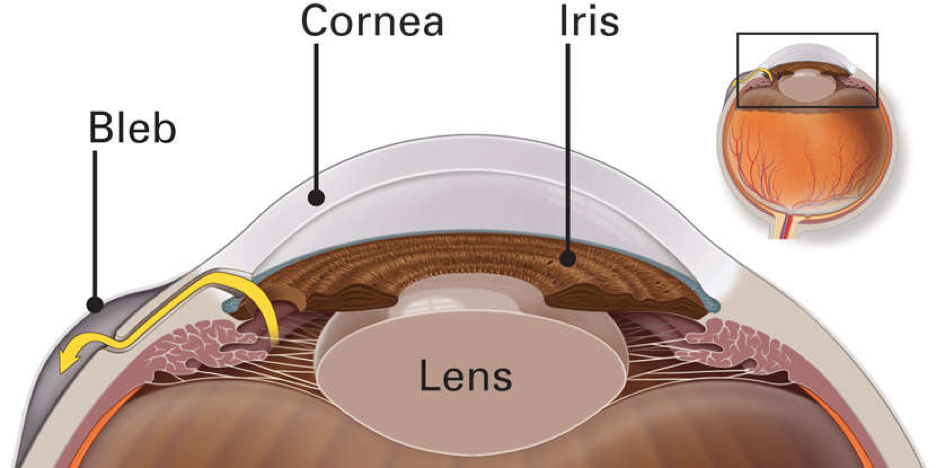
- Trabeculectomy
This is where your eye surgeon creates a tiny flap in the sclera. He or she will also create a bubble (like a pocket) in the conjunctiva called a filtration bleb. It is usually hidden under the upper eyelid and cannot be seen. Aqueous humor will be able to drain out of the eye through the flap and into the bleb. In the bleb, the fluid is absorbed by tissue around your eye, lowering eye pressure.
In trabeculectomy, a flap is first created in the sclera (the white part of the eye). Then a small opening is made into the eye to release fluid from the eye.
- Glaucoma drainage devices
Your ophthalmologist may implant a tiny drainage tube in your eye. The glaucoma drainage implant sends the fluid to a collection area (called a reservoir). Your eye surgeon creates this reservoir beneath the conjunctiva. The fluid is then absorbed into nearby blood vessels.
- Cataract surgery
For some people with narrow angles, removing the eye's natural lens can lower eye pressure. With narrow angles, the iris and the cornea are too close together. This can cover (block) the eye’s drainage channel. Removing the eye's lens with cataract surgery creates more space for fluid to leave the eye. This can lower eye pressure.
Your Role in Glaucoma Treatment
Treating glaucoma successfully is a team effort between you and your doctor. Your ophthalmologist will prescribe your glaucoma treatment. It is up to you to follow your doctor’s instructions and use your eye drops.
Once you are taking medications for glaucoma, your ophthalmologist will want to see you regularly. You can expect to visit your ophthalmologist about every 3–6 months. However, this can vary depending on your treatment needs.
If you have any questions about your eyes or your treatment, talk to your ophthalmologist.
Cataracts
A Cataract is a clouding of the natural lens inside the eye, hindering the eye’s ability to focus properly. The natural lens is made of a protein material that starts out clear and flexible and can change shape, allowing the eye to see clearly in a variety of distances.
Over time, the proteins in the natural lens break down making it less flexible and progressively cloudy. This process interferes with our ability to see both distance and near, and it can seem like looking through a foggy or dusty car windshield. Things look blurry, hazy or less colorful with a cataract.
Common Symptoms of Cataracts include:
- Gradually worsening blurry vision
- Seeing double or a ghosted images
- Problems with glare - Being extra sensitive to light (especially with oncoming headlights at night)
- Having trouble seeing well at night, or needing more light when you read
- Bright colors seem faded or yellow
- Low contrast print or images become more difficult to see
If you notice any of these cataract symptoms, notify the ophthalmologist.
What Causes Cataracts?
Aging is the most common cause. This is due to normal eye changes that begin to happen after age 40. That is when normal proteins in the lens start to break down. This is what causes the lens to get cloudy. People over age 60 usually start to have some clouding of their lenses. However, vision problems may not happen until years later.
Other reasons you may get cataracts include:
- having parents, brothers, sisters, or other family members who have cataracts
- having certain medical problems, such as diabetes
- smoking
- having had an eye injury, eye surgery, or radiation treatments on your upper body
- having spent a lot of time in the sun, especially without sunglasses that protect your eyes from damaging ultraviolet (UV) rays
- using certain medications such as corticosteroids, which may cause early formation of cataracts.
Most age-related cataracts develop gradually. Other cataracts can develop more quickly, such as those in younger people or those in people with diabetes. Doctors cannot predict how quickly a person’s cataract will develop.
You may be able to slow down your development of cataracts.
Protecting your eyes from sunlight is the best way to do this. Wear sunglasses that screen out the sun’s ultraviolet (UV) light rays. You may also wear regular eyeglasses that have a clear, anti-UV coating. Talk with your eye doctor to learn more.
Diagnosing Cataracts
The professionals at the Orchard Eye Center will examine and test your eyes to make a cataract diagnosis. This comprehensive eye exam will include dilation (eye drops to widen your pupils).
The Exam
Slit-lamp exam
Dr. Hillam will utilize a slit-lamp microscope to examine your cornea, iris, lens and the other areas at the front of the eye. This special microscope makes it possible to spot abnormalities.
Retinal Exam
Once your eye is dilated, the pupils stay wide open so the doctor can more clearly see the back of the eye. Using the slit lamp, an ophthalmoscope or both, the doctor looks for signs of cataract. Your ophthalmologist will also look for glaucoma, and examine the retina and optic nerve.
Refraction and visual acuity test
This test assesses the sharpness and clarity of your vision. Each eye is tested individually for the ability to see letters of varying sizes.
Diagnostic Testing
Specialized state-of-the-art ophthalmic testing equipment is often used during the exam to determine the extent of the effects of cataracts.
What to do if you are diagnosed with Cataracts:
- Have an eye exam every year if you're older than 65, or every two years if younger.
- Protect your eyes from UV light by wearing sunglasses that block at least 99 percent UV and a hat.
- If you smoke, quit. Smoking is a key risk factor for cataracts.
- Use brighter lights for reading and other activities. A magnifying glass may be useful, too.
- Limit driving at night once night vision, halos or glare become problems.
- Take care of any other health problems, especially diabetes.
- Get the right eyeglasses or contact lenses to correct your vision.
- When it becomes difficult to complete your regular activities, consider cataract surgery.
Make an informed decision about cataract surgery. Have a discussion with the ophthalmologist about:
- the surgery,
- preparation for and recovery after surgery,
- benefits and possible complications of cataract surgery,
- cataract surgery costs,
- other questions you have.
Cataract Treatment
To treat cataracts, the cloudy natural lens material must be removed. Cataracts can only be removed with surgery.
Cataract surgery is usually not urgent. If your symptoms are not bothering you very much, you don’t have to have the cataract removed. As they progress, cataracts often change your eyeglass prescription requirement and you might just need an updated eyeglass prescription to help you see better. You should consider surgery when cataracts interfere with doing the things you want or need to do.
What does Cataract Surgery involve?
Modern medical advancements and skill utilized by Dr. Hillam and his team make cataract surgery relatively straightforward for the patient. It is a short outpatient surgery requiring minimal aftercare.
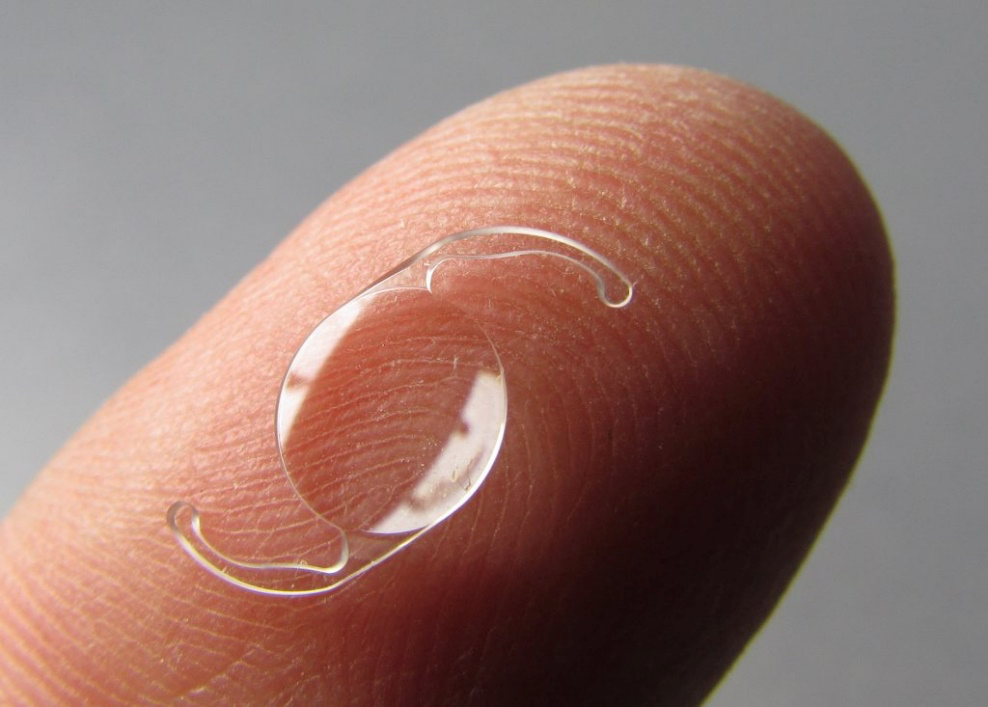
Simply put, during cataract surgery, Dr. Hillam removes your eye’s cloudy natural lens. Then he replaces it with a new man-made artificial lens that will last the lifetime of the patient. This new lens is called an intraocular lens (or IOL). When you decide to have cataract surgery, we will discuss with you the different IOLs available, how they work, and how to select the IOL best suited to your eye, circumstances, and desired outcome.
Can Cataracts come back after cataract surgery?
People who have had cataract surgery may have their vision become hazy again months or even years later. This is often because the clear membrane capsule of the eye (the structure of the eye which holds the lens/IOL in place) has now become cloudy. Dr. Hillam can utilize a simple laser procedures to open the cloudy capsule and restore clear vision. This is called a capsulotomy.
Cataracts are a very common reason people lose vision, but thanks to modern medical advances, current medical technology, and skilled professionals, cataracts are very much treatable!. You should discuss your cataract symptoms with Dr. Hillam and his professional team at the Orchard Eye Center. Together you can decide whether you are ready for cataract surgery.
Age-Related Macular Degeneration (AMD)
Age-related macular degeneration (AMD) is very common. It is a leading cause of vision loss in people 50 years or older. AMD is a disease process that effects the area of the Retina called the Macula. The Retina is a delicate layer of nerve tissue that lines the inside of the back of the eye that is responsible for vision, much like the film in a classic camera. The Macula is the portion of the Retina responsible for central detailed vision. AMD causes deterioration and loss of central vision and affects ability to see fine details, in both distance and near vision. Peripheral (side) vision is generally unaffected by AMD. For instance, imagine you are looking at a clock with hands. With AMD, you might see the clock’s numbers but not the hands. There are two Types of AMD – they are commonly dubbed “Dry AMD” and “Wet AMD”.
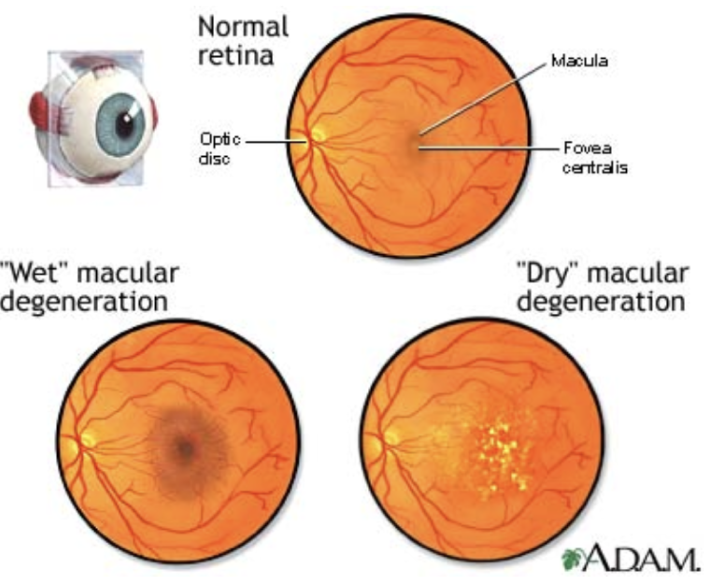
Dry AMD is quite common. About 80% (8 out of 10) of people who have AMD have the dry form. Dry AMD is typically less aggressive and slower progressing than Wet AMD. With Dry AMD, parts of the macula break down and get thinner with age and tiny clumps of protein called drusen grow within the retina. Many people with AMD have drusen, and these alone do not cause vision loss. But when drusen grow in size or number, you are at risk for getting early or intermediate AMD. There are not always symptoms with these stages of AMD, though people with intermediate AMD often start to notice a blurred spot in their central vision. Advanced Dry AMD develops when cells in your macula begin to break down. This process causes a slow gradual loss of central vision, and causes the blurred spot in the central vision to get bigger and darker. Currently, there are no successful treatments for Dry AMD.
Wet AMD is less common but much more serious. With Wet AMD, new abnormal blood vessels grow under the retina. These vessels are weak and often leak blood or other fluids, causing swelling and scarring of the macula. Vision loss is much faster with wet AMD than with dry AMD. Fortunately, there are some very successful treatments that help control Wet AMD. Unfortunately, many people don’t realize they have AMD until they experience dramatic vision loss and blurriness. Treatment can achieve some recovery of vision loss, but is meant to minimize progression of the disease and preserve remaing vision. This is why it is important to have regular visits to an ophthalmologist. An Ophthalmologist can detect early signs of AMD before you experience devastating vision loss from it, and may be able to treat the condition to preserve as much functional vision as possible.
Who Is at Risk for AMD?
No one knows exactly what causes dry macular degeneration. But research indicates it may be affected by a combination of heredity and environmental factors, including smoking, obesity and diet. AMD is more common in individuals who smoke, have a diet high in saturated fat, are Caucasian, are overweight, have high blood pressure, and are over 50 years of age. Heart disease and high cholesterol levels are also risk factors.
Age-Related Macular Degeneration Diagnosis
AMD can be diagnosed with a complete dilated eye exam. The professionals at the Orchard Eye Center utilize cutting-edge technology along with proven detection methods to diagnose AMD. The Ophthalmologist will look inside your eye with special lights and magnifying lenses, where changes in the retina and macula can be seen.

Optical coherence tomography (OCT) is a machine using highly-advanced technology to perform a scan of the retina and provide very detailed images of the retina and macula.
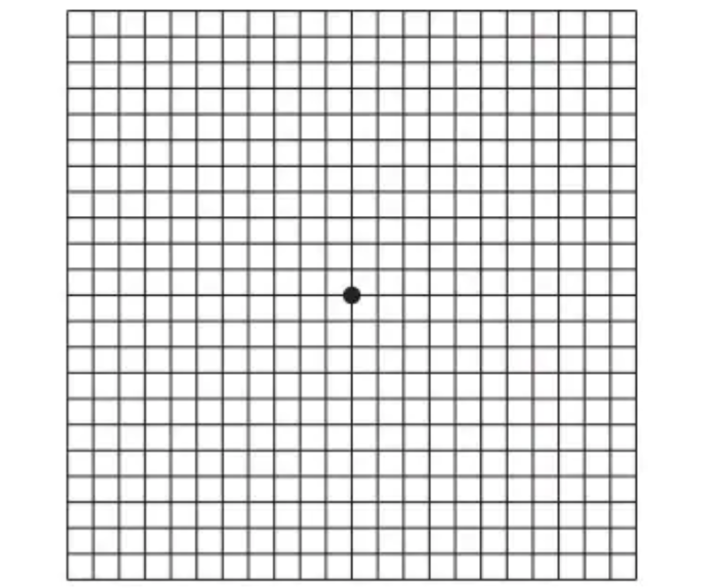
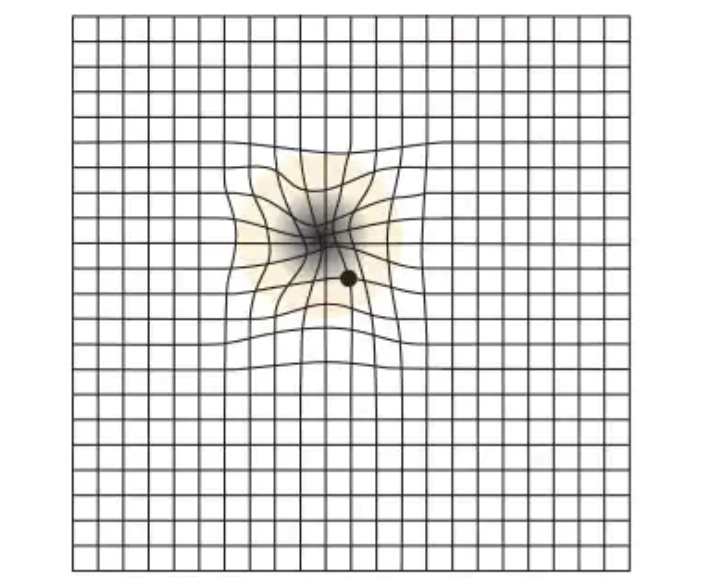
During the exam, you may also be asked to look at an Amsler grid. This grid helps you detect blurry, distorted, or blank spots in your field of vision. You may also be instructed how to use the Amsler Grid at home to detect progression or changes in visual defects.
Treatment for AMD
Eye-healthy foods
Dark leafy greens, yellow and red fruits and vegetables, fish, and a balanced, nutrient-rich diet have shown to be beneficial for people with AMD.
Dry AMD currently has no proven treatment. However certain people with many drusen or serious vision loss may benefit from taking a certain combination of nutritional supplements. AREDS 2 (Age-Related Eye Disease Study 2) was a very large research study that looked at taking vitamins and minerals daily for AMD. This study found that certain nutritional supplements could help slow the progression with certain types of Dry AMD, as well as reduce the chance of it becoming the more devastating Wet AMD. Your ophthalmologist can tell you if vitamins and minerals are recommended for your type of Dry AMD, as not all forms will benefit from the AREDS 2 supplements.
Wet AMD can now be treated with medications called anti-VEGF drugs. Anti-VEGF treatment helps reduce the number of abnormal blood vessels in your retina, and slows leaking from blood vessels. This makes it possible to reduce the harmful fluid and swelling which causes vision loss. This medicine is delivered to the inside of the eye using a tiny needle. To prepare for the injection, the doctor uses modern numbing methods and patients tolerate the experience quite well.
Making the Most of the Vision You Have
If you experience dramatic vision loss from AMD, you can learn how to make the most of your vision. Often you can still do many of your favorite things with special low vision tools. These can include different kinds of magnifying tools, handheld computers, electronic items and more.
Also, you can learn how to use your side vision to help you do things. A vision rehabilitation specialist can teach you how this works, and also help you find low vision support services and tools.
Ask your ophthalmologist to help you find a vision rehabilitation specialist in your area. The goal is to learn new ways to be as independent as possible.
What We Offer
Comprehensive Eye Care Services
Our facilities are equipped with state-of-the-art ophthalmic technology to provide the most effective treatment.

Cataract Surgery
Detail oriented cataract surgery – Because your vision matters to us

Intravitreal Injections
Up-to-date treatment for ocular disease

Comprehensive Exams
We are here to help you experience vision at its fullest

Urgent Care
When you are worried about your eyes, call us right away
Don't hesitate, contact us to learn more about our services